How Abnormal Blood Flow Drives Brain Fog and Fatigue in POTS and ME/CFS
If you're living with POTS or ME/CFS, you know brain fog all too well. That frustrating mix of trouble focusing, mental cloudiness, and overwhelming exhaustion that makes thinking feel like walking through mud. For a long time, medical and allied health practitioners have struggled to measure and explain what you're experiencing. Recent research has given us concrete evidence that brain fog is real, and happens when your brain doesn't get enough blood flow, a condition called cerebral hypoperfusion (Khan et al., 2025; Seeley et al., 2025).
What scientists are discovering is that problems with blood flow to the brain are a fundamental issue shared across many types of dysautonomia, particularly those involving orthostatic intolerance (when your body struggles with position changes). These symptoms can be so life altering that people with orthostatic intolerance often experience quality of life similar to those living with serious conditions like severe heart failure (Khan et al., 2025).
What's Actually Happening: Your Brain's Blood Flow Regulation Isn't Working Properly
Your brain needs a constant, steady supply of oxygen and nutrients to function. To make this happen, it has a built-in protection system called cerebral autoregulation. Think of it as a thermostat that keeps your brain's blood flow stable even when your overall blood pressure changes.
For many people with POTS, this system breaks down when standing up (Medow et al., 2014). Research using tilt table tests shows that when blood pressure becomes unstable and starts fluctuating in wave-like patterns (called Mayer waves), the blood flow to the brain starts fluctuating right along with it (Medow et al., 2014). Instead of staying steady like it should, the brain's blood flow essentially rides these unstable waves of blood pressure. This happens because the brain's ability to smooth out these fluctuations is impaired. These dramatic swings in blood flow may directly cause the cognitive problems—the brain fog, confusion, and difficulty thinking—that you experience when upright (Medow et al., 2014).
It's Not Just When You're Standing: The Problem Exists While Sitting and Lying Down Too
One revealing study looked at what happens during mentally demanding tasks while seated. POTS patients experienced a much larger drop in blood flow to the brain (nearly 8%) compared to healthy people (less than 2%) (Wells et al., 2020).
This decrease was enough to cause measurably slower thinking and increased difficulty concentrating (Wells et al., 2020). What's particularly striking is that the drop in brain blood flow during mental tasks was about the same size as what happens when standing up—meaning cognitive effort alone can trigger significant reductions in blood flow.
The Evidence Is Becoming Obvious
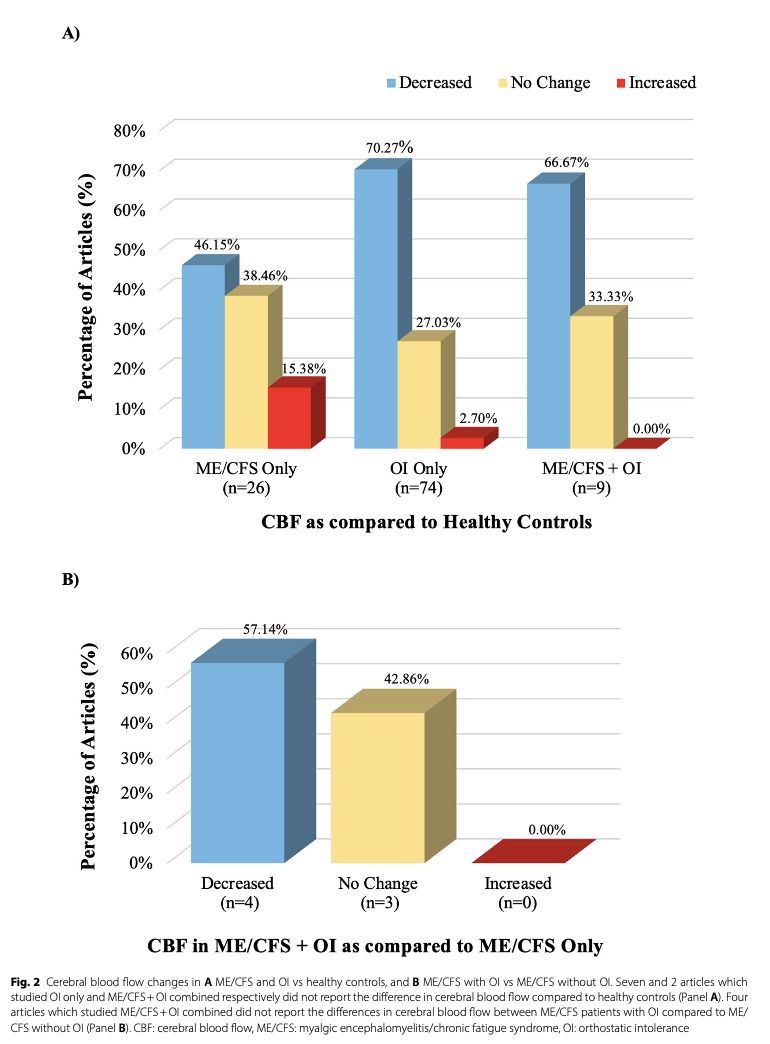
A very recent systematic review analyzed 118 studies involving over 9,000 participants with ME/CFS and orthostatic intolerance found significantly reduced brain blood flow in both ME/CFS patients (12 out of 26 studies) and those with orthostatic intolerance (57 out of 81 studies) compared to healthy people (Christopoulos et al., 2025).
What's particularly revealing is what happens when you have both conditions together. In studies that looked at people with both ME/CFS and orthostatic intolerance, four out of seven found that having both conditions led to even greater reductions in brain blood flow than having ME/CFS alone (Christopoulos et al., 2025). This suggests that when these conditions occur together, they may amplify each other's effects on your brain, potentially explaining why symptoms can be so severe.
Even more compelling, advanced brain imaging (using a technique called SPECT scanning) on POTS patients with cognitive symptoms found that 61% showed abnormal blood flow even while lying flat (Seeley et al., 2025). The areas getting the least blood were the lateral prefrontal and sensorimotor regions (Seeley et al., 2025). These brain areas are crucial for executive function, planning, memory, and attention—directly connecting the physical lack of blood flow to the brain fog symptoms you experience (Seeley et al., 2025).
The systematic review confirmed these patterns across multiple imaging techniques and testing conditions (Christopoulos et al., 2025). Whether researchers measured blood flow while patients were lying down, sitting, or standing, the pattern remained consistent: reduced blood flow to the brain is a core feature of both conditions.
Why Traditional Testing Often Misses the Diagnosis
This focus on brain blood flow is vital because relying solely on traditional measurements—heart rate and blood pressure—to diagnose orthostatic intolerance often isn't enough and leads to people being told they're fine when they're not (Khan et al., 2025).
Studies using specialized imaging that measures total blood flow to the brain (not just velocity) in ME/CFS patients during tilt table testing found an average reduction in brain blood flow of 26%—far more than the 7% reduction seen in healthy people (van Campen et al., 2020). Here's the most important finding: 82% of ME/CFS patients who had completely normal heart rate and blood pressure during the test still showed abnormally reduced brain blood flow (van Campen et al., 2020).
This reveals a critical gap in how these conditions are diagnosed. Without measuring brain blood flow directly, somewhere between 22% and 58% of people with genuine orthostatic intolerance symptoms risk being told their test results are "objectively normal" when their brain is actually not getting enough blood (Khan et al., 2025). The systematic review reinforced this finding, showing that across dozens of studies, many patients experience significant brain blood flow problems despite having normal vital signs (Christopoulos et al., 2025).
Additionally, researchers found that the worse someone's symptoms during the tilt test—including fatigue, leg muscle weakness, and concentration problems—the greater their reduction in brain blood flow (van Campen et al., 2020). Your symptoms aren't "all in your head"—they directly correspond to measurable changes in how much blood your brain is receiving.
The Mechanical Factor: Brain Vessel Stiffness
Beyond how blood flow is regulated, the physical properties of your brain's blood vessels may also play a role. Research on Chronic Fatigue Syndrome patients looked at something called intracranial compliance—essentially how well the brain's vascular system can mechanically absorb and buffer pressure changes with each heartbeat (Finkelmeyer et al., 2018).
While CFS patients and healthy people didn't differ significantly in overall compliance or blood flow at rest, researchers found something interesting within the patient group: those reporting more severe orthostatic intolerance symptoms tended to have lower intracranial compliance (Finkelmeyer et al., 2018). Lower compliance might mean the brain's blood vessels are less able to dampen blood pressure fluctuations, particularly rapid ones, potentially making it harder for the brain to maintain steady blood flow and worsening orthostatic intolerance symptoms (Finkelmeyer et al., 2018).
What This Means for Diagnosis and Treatment
The evidence is now overwhelming. Multiple measurement techniques, thousands of patients studied, and consistent findings across research groups all point to the same conclusion: brain fog and fatigue in POTS and related orthostatic intolerance conditions are the direct result of insufficient and unstable blood flow to the brain (Christopoulos et al., 2025). This often happens even when heart rate and blood pressure appear normal.
Measuring cerebral blood flow is therefore an essential, objective marker that validates what you're experiencing and should be part of how doctors diagnose and treat people with dysautonomia, especially those with orthostatic intolerance. As the research community continues to recognize this, we're moving toward better diagnostic tools and more targeted treatments that address the root cause rather than just managing symptoms.
If you’d like help managing POTS, ME/CFS or Dysautonomia, submit a message or enquiry here.
REFERENCES:
Christopoulos, E. M., Tantanis, D., Huang, K., Schneider-Futschik, E. K., Gooley, P. R., Moneghetti, K. J., & Armstrong, C. W. (2025). Mapping cerebral blood flow in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and orthostatic intolerance: insights from a systematic review. Journal of Translational Medicine, 23, 963. https://doi.org/10.1186/s12967-025-06954-w
Finkelmeyer, A., He, J., Maclachlan, L., Blamire, A. M., & Newton, J. L. (2018). Intracranial compliance is associated with symptoms of orthostatic intolerance in chronic fatigue syndrome. PLoS ONE, 13(7), e0200068. https://doi.org/10.1371/journal.pone.0200068
Khan, M. S., Miller, A. J., Ejaz, A., Molinger, J., Goyal, P., MacLeod, D. B., Swavely, A., Wilson, E., Pergola, M., Tandri, H., Frazier Mills, C., Raj, S. R., & Fudim, M. (2025). Cerebral blood flow in orthostatic intolerance. Journal of the American Heart Association. Advance online publication. https://doi.org/10.1161/JAHA.124.036752
Medow, M. S., Del Pozzi, A. T., Messer, Z. R., Terilli, C., & Stewart, J. M. (2014). Altered oscillatory cerebral blood flow velocity and autoregulation in postural tachycardia syndrome. Frontiers in Physiology, 5, 234. https://doi.org/10.3389/fphys.2014.00234
Seeley, M. C., O'Brien, H., Wilson, G., Coat, C., Smith, T., Hickson, K., Casse, R., Page, A. J., Gallagher, C., & Lau, D. H. (2025). Novel brain SPECT imaging unravels abnormal cerebral perfusion in patients with postural orthostatic tachycardia syndrome and cognitive dysfunction. Scientific Reports. Advance online publication. https://doi.org/10.1038/s41598-025-87748-4
van Campen, C. M. C., Verheugt, F. W. A., Rowe, P. C., & Visser, F. C. (2020). Cerebral blood flow is reduced in ME/CFS during head-up tilt testing even in the absence of hypotension or tachycardia: A quantitative, controlled study using Doppler echography. Clinical Neurophysiology Practice, 5, 50–58. https://doi.org/10.1016/j.cnp.2020.01.003
Wells, R., Malik, V., Brooks, A. G., Linz, D., Elliott, A. D., Sanders, P., Page, A., Baumert, M., & Lau, D. H. (2020). Cerebral blood flow and cognitive performance in postural tachycardia syndrome: Insights from sustained cognitive stress test. Journal of the American Heart Association, 9(22), e017861. https://doi.org/10.1161/JAHA.120.017861